Blog Categories
Free Consultation
By submitting this form and signing up for texts, you consent to receive informational text messages from The Orlow Firm at the number provided, including messages sent by the auto dialer. Consent is not a condition of purchase. Msg & data rates may apply. Msg frequency varies. Unsubscribe at any time by replying STOP. Reply HELP for help. Privacy Policy
Our Reviews on google
The Orlow Firm's Reputation On Google
The Orlow Firm is rated 4.9/5 across all of our Google reviews (as of May 2025). Below is a small sample of what people are saying about the firm and the compassionate advocacy we provided for them.
Prior results do not guarantee a similar outcome.
I’m very thankful because of the Orlow firm won my case , trustable , every time I had a question they would respond.
Thank you lawyer Bryan for helping me with my case.
Since I have my accident
Brain Orlow and his team
Been helping me every step with case
They. Are concerned about client
Make sure they have good access to doctors appointments
And financial support
For me i will hire this firm again
Memberships & Accolades
The Orlow Firm's Accolades
Established in 1982, The Orlow Firm has earned numerous accolades for its dedication to client advocacy and legal excellence. These recognitions reflect our unwavering commitment to achieving justice, delivering results, and providing compassionate, personalized representation to injury victims throughout New York City. Our reputation has been built on decades of trust, integrity, and a tireless pursuit of the best possible outcomes for those we serve. We’re proud to be recognized not just for our results, but for the care and respect we show every client.
Attorney Advertising: No aspect of these accolades has been approved by the New York State Court of Appeals.






Client testimonials
The Orlow Firm's Results Speak for Themselves.
Prior results do not guarantee a similar outcome.

Submit your review | |
1 2 3 4 5 | |
Submit Cancel | |
I was involved in a car accident and sustained some serious injuries. I got in touch with The Orlow Firm and spoke to Brian. I couldn't have been happier with the results. I was always made to understand the decisions I needed to make, they were very flexible and patient with me and I truly believe they got me the most compensation possible due to their experience and knowledge. I recommend them to anyone looking for a personal injury firm in New York.
Submit your review | |
1 2 3 4 5 | |
Submit Cancel | |
I am thrilled with the results of my case. I highly recommend The Orlow Firm to any and all that are in need of a personal injury lawyer in NYC.
We had a situation where my mother had been neglected in a nursing home and the injuries were appalling. The Orlow Firm comforted us, knew what steps to take and got us the justice we deserved for our mother. I will be forever grateful to them for their compassion and hard work.
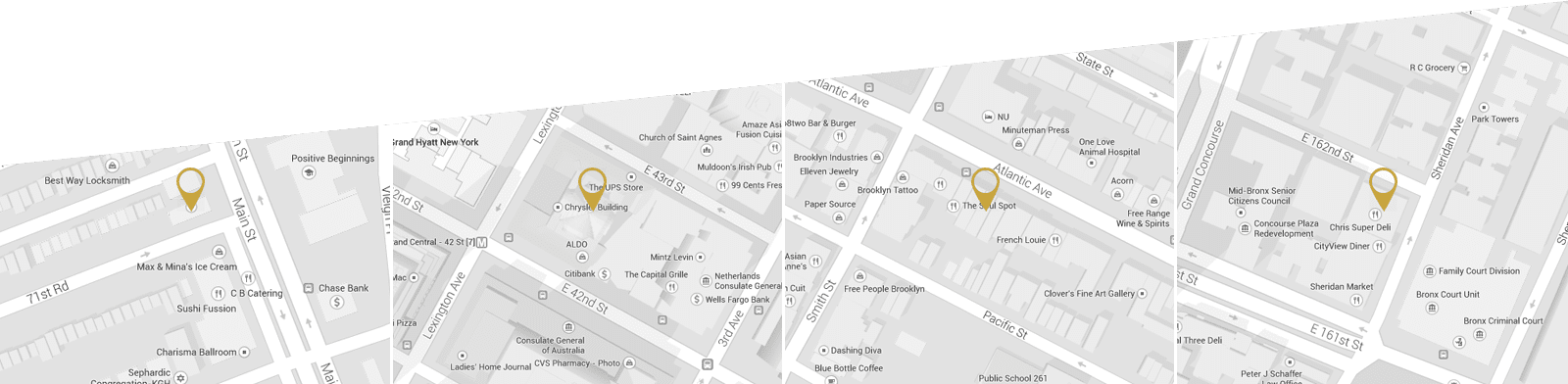
Our Locations
We offer free initial consultations and operate four offices across New York City for your convenience. We can go to you if you cannot come to us.
Queens Law Office
71-18 Main Street
Queens NY 11367 Map
(646) 647-3398
Fax: 718-544-6485
Manhattan Law Office
(by appointment only)
The Chrysler Building, 26th Floor
405 Lexington Ave
New York NY 10174 Map
(646) 647-3398
Fax: 718-544-6485
Brooklyn Law Office
(by appointment only)
32 Court Street
Brooklyn NY 11201 Map
(646) 647-3398
Fax: 718-544-6485
Bronx Law Office
(by appointment only)
903 Sheridan Avenue
2nd Floor
Bronx, NY 10453 Map
(646) 647-3398
Fax: 718-544-6485
We can help you! Request a free consultation.
The Orlow Firm represents injured people in the five boroughs of New York City (Manhattan, Brooklyn, Queens, The Bronx and Staten Island) as well as the counties surrounding New York City.
Attorney Advertising Disclaimer
Notice: The information on this website is for general information purposes only. Nothing on this site should be taken as legal advice for any individual case or situation. This information is not intended to create, and receipt or viewing does not constitute, an attorney-client relationship. Prior results do not guarantee a similar outcome. The Orlow Firm works on a contingent fee basis. A contingent basis means that our attorneys do not charge by consultation but will take a percentage on the amount recovered. This amount is usually one third of the net recovery after disbursement. This means that the cost of hiring The Orlow Firm varies based on the amount recovered.
© 2025 by the The Orlow Firm. All Rights Reserved. Privacy Policy. Terms & Conditions.
